A Roadmap for Workforce Training to Meet the Needs of Patients with Serious Illness

We Do What We’re Trained to Do
People living with serious illness assume – reasonably – that their clinicians have the training it takes to help them cope with their illness. But what does this ‘help’ mean?
If I have cancer, I will certainly get help fighting it with drug therapies or procedures But if during treatment I have pain or am exhausted, will my clinicians ask me about it, and then help me manage my symptoms? When my tests come back, will my clinician know how to break the news compassionately, so that I’m not traumatized? If at times, my spouse is in worse shape than me, and I’m not sure how we’ll get to the pharmacy for our refills, does anyone on my care team know to ask or to coordinate a delivery?
Palliative care specialists focus their time on addressing these questions – and their skills are badly needed when patients’ symptoms, decisions, and lives become acutely complicated during a serious illness. But whether a patient is being seen by a palliative care specialist, their primary care doctor, or a nurse practitioner (NP) at the cancer clinic, we have an opportunity to provide better care in every clinical interaction by routinely assessing and addressing patients’ palliative care needs.
Why doesn’t this happen already? Most clinicians simply haven’t been trained.
Health care professionals cannot be expected to provide what they have never been trained to do. The result of this can be unnecessary suffering, reduced quality of life, and higher health care costs for the people living with a serious illness (and their families), who are under their care.
Palliative Care Education for All Clinicians
That’s why the National Consensus Project’s Clinical Practice Guidelines for Quality Palliative Care, 4th edition (NCP Guidelines) outline the skills that all clinicians need in order to care for people with serious illness – from any discipline, specialty, and care setting. The NCP Guidelines are the gold standard for palliative care quality; when the latest edition was published in 2019, it was the first time that palliative care services every clinician can and should provide to their patients was defined.
The NCP’s recommendations fall into four important skill sets that are addressed in CAPC’s new training recommendations:
- Assessing the needs and concerns of patients: Beyond best practice disease management, how can clinicians understand what each patient needs to avoid crises and live as well as possible with their diagnosis?
- Strengthening the clinician-patient relationship and understanding care goals: What matters most to the patient in the context of their illness, and how can clinicians establish the trusting relationship needed to navigate difficult care decisions?
- Managing pain and symptoms: What are the most common symptoms experienced by patients with serious illness, and which symptom management strategies are effective?
- Preventing crises and helping patients plan ahead: Can clinicians connect patients with the information and resources needed to meet their changing needs, honor their changing priorities over time, and to live safely at home, if that is their goal?
A National Trend
A growing number of health care organizations across the country have begun using clinical training as a tool to improve the quality of care for patients living with a serious illness. CAPC has seen remarkable growth year over year, in the number of clinicians (who are not palliative care specialists) using our online continuing education (CE) curriculum to learn core palliative care skills – and our colleagues from other training organizations such as the End-of-Life Nursing Consortium (ELNEC) and VitalTalk report the same. In November 2019, the National Academies of Sciences, Engineering, and Medicine (NASEM) hosted a day-long workshop that highlighted palliative care education for non-palliative care specialists as a key strategy to prepare the U.S. health care workforce to meet the needs of the growing number of people living with serious illness.
"A growing number of health care organizations across the country have begun using clinical training as a tool to improve the quality of care for patients living with a serious illness."
Now, in the midst of COVID-19, the need for this training is even clearer.
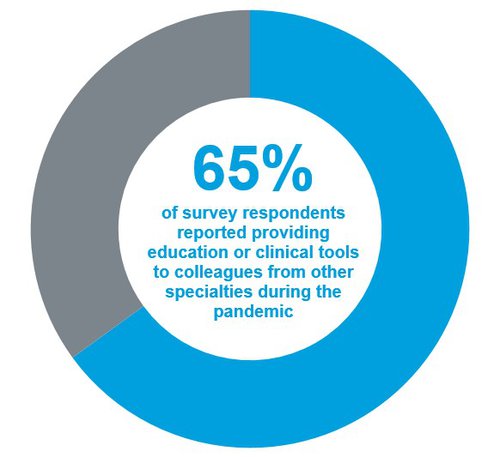
In national survey conducted by CAPC in May 2020, 65% of palliative care programs reported providing clinical education (including communication scripts and symptom management guidance) to colleagues from other specialties, since the beginning of the pandemic. This upward trend needs to continue, as our patient population is growing.
How Health Care Organizations Can Take Action
We’ve made the case that additional training is important. The NCP Guidelines, referenced earlier, tell us what skills all clinicians need, to care for patients with serious illness (e.g. communication skills and symptom management) – and there are a number of high-quality education options to choose from. How should health care organizations use this information and sort through the options, in order to design a training program for their clinicians?
To make this process easier, CAPC recently published specific training recommendations for clinicians from all disciplines – including pediatric and adult providers – based on guidance from the NCP Guidelines.
CAPC's training recommendations do two things:
- List the specific skills that all clinicians need in order to improve care for people living with a serious illness; they are broken down by discipline and include physicians, advanced practice providers, registered nurses, social workers, chaplains, and clinical care managers
- Identify available CAPC courses and tools that clinicians and health care organizations can use to ensure standardized training; the goal is to develop the knowledge and skills required to care for people living with a serious illness, and their families
Many health care organizations are already taking steps to equip their clinicians with the knowledge and skills needed to strengthen care – and improve outcomes – for people with serious illness. We hope that CAPC’s new training recommendations provide an easy-to-follow roadmap so that every health system, hospital, community-based provider, and health plan joins in the effort to ensure a well-prepared workforce.
"We hope that CAPC’s new training recommendations provides an easy-to-follow roadmap so that every health system, hospital, community-based provider, and health plan joins in the effort to ensure a well-prepared workforce."
In Conclusion
If every clinician in the U.S. were trained in the fundamentals of communication, symptom management, and family caregiver support skills, would we still need palliative care specialists? Yes, as palliative care specialists are experts in supporting patients and families whose needs are most complex. But every patient living with a serious illness expects and deserves care from clinicians who can meet their most fundamental human needs – and who can see and respond to their suffering. If all clinicians are trained in these core skills, we will be able to provide better and more compassionate care for our patients.
"If all clinicians are trained in these core skills, we will be able to provide better and more compassionate care for our patients."
Available by discipline, the new training recommendations help clinicians and health care organizations address the unique needs of patients living with serious illness.
Get Started
