How to Build Bridges Between Palliative Care and Rehabilitation Teams
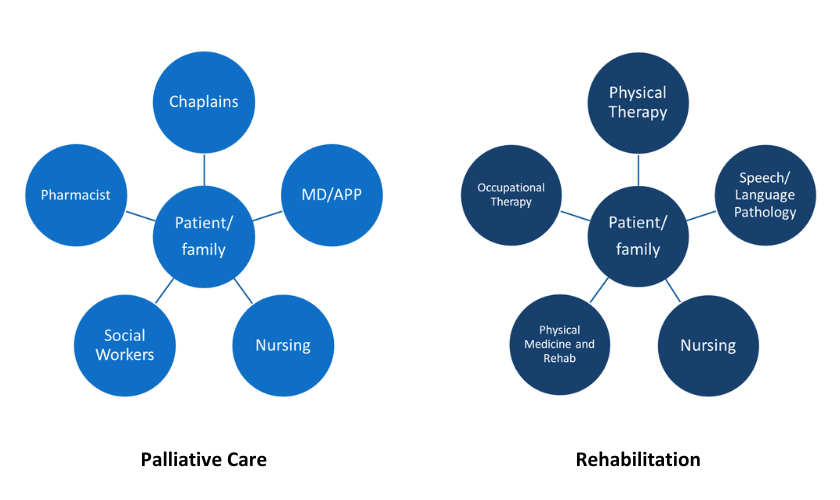
If you’ve consulted with an occupational therapist (OT), physical therapist (PT), or speech-language pathologist (SLP), you may have noticed that their objectives closely mirror those of the palliative care team. These rehabilitation professionals (also known as rehab therapists) are dedicated to improving the quality of life and functional independence of people living with serious illness, and their families. They assess personal goals and values, manage symptoms, and facilitate participation in meaningful activities throughout the disease trajectory. However, despite their shared objectives, both teams often work in parallel rather than tandem.
"... You may have noticed that [rehabilitation therapy's] objectives closely mirror those of the palliative care team."
Wouldn’t it be better if these teams collaborated? We, the authors of this blog—a palliative care physician and an occupational therapist from MedStar Georgetown University Hospital—believe so. The World Health Organization (WHO) concurs. In an April 2023 policy brief, the WHO emphasized that palliative rehabilitation services are a right for patients. They assert that rehabilitation and palliative care services are essential for quality health care and should be integrated into health systems in a multi-professional manner.
While this integration poses challenges in the current health care environment, it is essential for the provision of quality care for people with serious illness, and their families.
For the past few years, the rehabilitation therapy and palliative care teams at MedStar Georgetown University Hospital have been working to connect these teams more efficiently and effectively, ultimately improving care for people living with serious illness, and their families. We’re excited to share our story and the lessons we’ve learned.
What We've Learned From Our Palliative Care and Rehabilitation Therapy Collaboration
When our teams started working together, we first examined barriers to collaborative practice using IPEC Core Competencies as a framework. Interprofessional collaboration is challenging for many reasons, such as inadequate educational preparation, the historically siloed structure of the US health care system, resource constraints, productivity demands, and role misunderstandings.
The success of our teams' ongoing collaboration is due to the values below, which address these barriers and foster a team-based culture.
1. Focus on cross-team education
At the start of our collaboration, both teams “in-serviced” each other to share perspectives and understand our unique roles in working with our patient population. This interprofessional sharing and later shadowing yielded incredible role clarity for all providers. Some key takeaways from this experience include:
Rehab therapists can provide mindfulness-based interventions (e.g., breathing exercises, meditation, etc.)
Mindfulness-based interventions help prepare for mobility, address anxiety, or augment pharmacological pain management interventions. Some free options include the UCLA Mindfulness app and the CBTi Coach from the VA. Fatigue management, energy conservation, and sleep hygiene are salient PT and OT goals for this population.
Discharging a person from the acute care setting to home hospice is a critical period for involving or re-engaging rehabilitation professionals
Family training and home equipment specifications can make a massive difference in quality of life at home. Consider a drop-arm bedside commode and/or wheelchair—and maybe a high-back reclining wheelchair or Geri-Chair in preparation for squat pivot transfers if standing becomes too difficult!
Speech-language pathologists are not just about thickened liquids
They can be valuable contributors during discussions about whether or not to tube feed and best practice for safe, comfort feeding.
2. Make palliative care rounds more accessible to rehab therapists
This means encouraging rehab therapists to attend palliative care rounds for specific patients instead of the entirety of the meeting and being flexible with the format. This is an ongoing challenge for us, given productivity demands and resource constraints.
3. Communicate beyond documentation
Documentation-sharing is limited communication. Our teams have explored optimizing how we use the EHR to enhance communication, which is a work in progress.
We asked ourselves how to ensure every provider has the same, up-to-date information about prognosis, illness communication, and plans. In response, we’ve started communicating through our hospital's chat system, Microsoft Teams (Teams), which allows us to connect in real time to share details.
How Our Palliative Care and Rehabilitation Therapy Collaboration is Evolving
Addressing the barriers to collaboration is an ongoing process at our organization. At the same time, we have capitalized on the facilitators to collaboration, namely our shared goals and complementary cultures across departments. To that end, we are continuing to grow and improve the following systems:
1. Engaging in real-time communication
Communication through Teams, text, or in-person has been an evolving process. We have found that the more we collaborate and get to know one another, the more effective the hallway/elevator chat becomes. We continue to consider specific palliative care order sets for therapy, EHR pop-ups to notify one another about status changes, or family meeting reminders. Texting and Teams chats seem to be the current winners in this quest for real-time communication.
2. Encouraging rehab therapists to make palliative care referral recommendations
Rehabilitation caseloads include patients receiving palliative care services, but many are not receiving this care. Rehab professionals often identify existential crises or unmet pain management needs across teams and settings for individuals not yet considered “appropriate” for palliative care. Empowering rehab professionals to request palliative care consults from the primary team expands the reach of a person-centered holistic care model.
"Rehab professionals often identify existential crises or unmet pain management needs across teams and settings for individuals not yet considered 'appropriate' for palliative care."
3. Improving discharge planning
Discharge planning is challenging for rehab therapists given often unknown prognosis/plans and availability of support in the home environment. However, after each visit, rehab therapists are tasked with providing a recommended discharge location (e.g., home with support, subacute rehab, or acute rehab).
Anticipated decline in function, cognitive deficits, and safety concerns are commonplace. A discharge recommendation by OT/PT is set at a point in time and generally reflects the safest disposition, given what is known about the plan and home set-up. Rehab therapists seek to match the values, goals, and desires of the person with serious illness (typically, these are to stay at home) and will work to create plans to match these values and wishes. Playing the role of a realistic cheerleader without instilling false hope in the concept of “going to rehab to get stronger” is a bit of a tightrope.
4. Requiring goals of care conversations training for all rehab therapists
Rehab professionals spend precious time with people with serious illness and are often privy to deep emotions and worries (“I am not sure I can fight anymore, but I know my family is counting on me” or “I am worried about my son, who will have to focus on my self-care needs when I go home”).
Many rehab therapists worry that goals of care conversations are not within their skillset or scope. To this end, we have begun training our rehab professionals on goals of care conversations, teaching specific skills to assess disease understanding, highlight values and preferences, and respond to difficult emotions.
To date, we have completed three training sessions, and preliminary results are positive. Equipping OT/PT and SLP team members with the tools and confidence to start these conversations benefits the entire care team and, more importantly, the patient.
"Equipping OT/PT and SLP team members with the tools and confidence to start these [goals of care] conversations benefits the entire care team and, more importantly, the patient."
5. Sharing the concept of “rehab in reverse” across the hospital (and to payers)
This concept is about creating a culture of helping people with serious illness decline with dignity, when improving function is no longer a realistic goal. This means shifting our focus from task performance to active participation in meaningful tasks, which will vary widely across individuals—some may want to don their own socks (and OT can certainly help!). Still, others may prefer to have family members complete this task and save energy for playing a game with their grandchild. This shift can impact the documentation of goals and clearly articulate the value of therapy services for reimbursement.
A Few Final Thoughts
This work is hard, and palliative care and rehabilitation professionals work tirelessly to ease suffering and enhance quality of life for our patients. That said, it is difficult to prioritize quality improvement work in the chaos of daily patient demands.
We urge you to identify interprofessional champions and give one another grace as you forge this journey. It will take longer than you may imagine, but that is okay; just keep moving toward the WHO vision: rehabilitation and palliative care services are essential to quality health care and should be integrated into health systems in a multi-professional manner. The end goal is worthy: high-quality, person-centered, holistic, coordinated care for all.
Resources
CAPC has developed clinical training recommendations for physicians, occupational therapists, physical therapists, speech-language pathologists, and other disciplines to address the unique needs of people living with serious illness. We recommend reviewing the training recommendations and using the associated Learning Pathways for the training and tools needed to acquire the new skills.

Be the first to read articles from the field (and beyond), access new resources, and register for upcoming events.
SubscribeEdited by Melissa Baron. Clinical review by Andrew Esch, MD, MBA.

