How to Support Your Organization’s Emotional PPE Needs during COVID-19
An Introduction
It is hard to overstate the negative impact of COVID-19 on health care professionals’ emotional well-being. The pandemic has placed enormous new burdens on a workforce that already had high burnout rates, with an estimated 35-60% of clinicians affected. Palliative care teams have found themselves on the front lines in new ways: redeployed to EDs or ICUs; standing up new telemedicine services in record time; seeing unprecedented numbers of patient deaths; and having to restrict family access. And since palliative care team members do not work or live in a bubble, they are also affected by myriad events occurring outside their organizations’ walls, including racial injustice, economic instability, widespread business and school closures, political tension, and environmental disasters.

Not knowing when or if circumstances will return to “normal” means that everyone must develop new and broader strategies to sustain well-being over time.
CAPC has curated many resources that palliative care professionals can use to promote emotional resilience for themselves and their teams. That said, the impact of individual and team wellness strategies is limited if organizations/institutions/employers fail to support the emotional well-being of their workforce. We spoke to health care leaders who take this idea of “Organizational Emotional PPE” seriously, augmenting existing services and developing new initiatives to support their clinical and non-clinical workers alike.
Palliative care teams are uniquely well-suited to support these organizational efforts, given communication skills, comfort with care of very sick people and their families, decision making under conditions of uncertainty (which has become the daily work of all clinicians in COVID-19 surges), and expertise in working with limited resources. Team members may feel drawn to participate or even lead these organizational efforts. To assist, this blog discusses promising organization-wide initiatives to promote well-being and resilience among clinical and non-clinical health care workers, and how palliative care teams can contribute to organizational efforts while retaining a primary focus on team and individual well-being.
Overview of Organizational Approaches to Emotional PPE
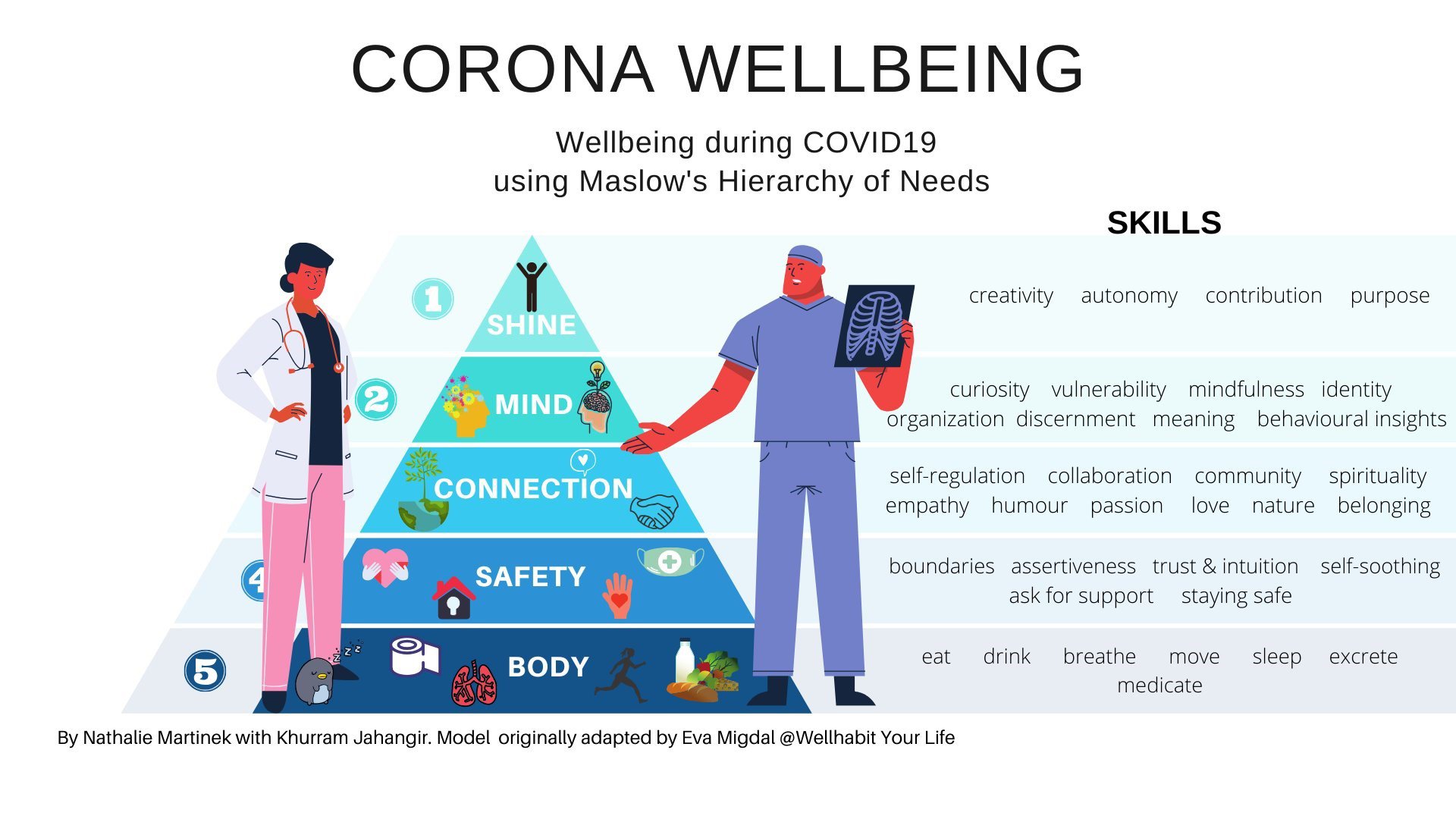
The organizations we spoke with learned early on that addressing concerns about safety – such as having sufficient PPE – was the essential prerequisite for emotional health. Only when these concerns were adequately addressed could staff “hear” the other supports that were available to them. An adaptation of Maslow’s Hierarchy of Needs for health care professional well-being during COVID-19, provides a helpful framework.
Important Lessons Shared by Leaders
- Efforts to support emotional PPE should focus both on the needs of clinicians, as well as the emotional impact on all health care workers. This means offering diverse programs and resources and availability for all shifts
- Given the numerous and complex sources of stress, it is important to have a solid understanding of what is in the organization’s sphere of influence when developing employee supports (for example, the hospital cannot control the cleanliness of public transportation, but can facilitate a carpool system)
- It can be helpful to survey employees to better understand specific concerns and better target interventions (example survey from The University of Texas Rio Grande Valley School of Medicine here)
- Embed wellness activities into existing workflows, and/or offer a variety of times to enhance accessibility
- It is important to acknowledge that sources of burnout that existed prior to COVID (e.g., EHR/documentation burden; RVU volume pressures) are still relevant and, in some cases, accelerate COVID-related burnout
- Health care professionals in need of mental health support often do not seek it. Reasons for this can be personal (e.g., not enough time, nature of the issue [e.g., depressive symptoms] might prevent outreach, shame) and/or systemic (e.g., stigma, payment, organizational demands, concern about professional repercussions, in-system mental health supports may flag in medical record). A recent NEJM article describes actions that organizations can take to reduce barriers for employees seeking help, such as:
- Establish and provide resources for peer support programs
- Conduct proactive outreach to employees who might need additional emotional support, using established triggers (e.g., the death of a colleague from COVID-19), rather than relying on self-referral
- Provide “reach in” psychological services that are free, easily accessible, and do not create risk for the employee seeking these services out
- Create processes to assess and address employees’ concerns, including soliciting feedback and taking transparent steps to respond to issues. Demonstrate accountability by investing resources in supporting the workforce and establishing metrics to track progress
- Many employees are suffering from “information overload”; therefore, disseminate resources strategically through a variety of channels (electronic, print, verbal announcements), and in easily digestible formats
- Tap into existing expertise when developing organization-wide emotional PPE support, including diversity and inclusion offices, behavioral health teams, and palliative care teams
Your organization’s capacity to provide a supportive environment may depend on size, resources, etc., and not all will be able to create/sustain comprehensive wellness initiatives. We strongly encourage organizations to leverage what has already been built; see CAPC’s Organizational Wellness page, as well as the list of resources at the bottom of the blog for more information.
"We strongly encourage organizations to leverage what has already been built."
The Palliative Care Team's Role
Palliative care teams understand the emotional/psychosocial side of caring and can play a role in larger system efforts, if they choose to do so. It may be that supporting organization-wide efforts to improve emotional PPE is a way to make meaning out of the pandemic, enhancing one’s own resilience. Palliative care teams can further demonstrate value to their organization by:
- Leading communication training efforts
- Sharing established materials/processes/procedures (e.g., an existing bereavement support protocol)
- Increasing awareness among colleagues about reliable availability of palliative care consultation services (e.g., through a telemedicine hotline)
- Highlighting the informal emotional support (“curbsiding”) that palliative care teams provide to colleagues
The decision to participate in organization-wide emotional PPE efforts should be based on a clear understanding of the team’s capacity and what its members can reasonably expect to contribute. The fact is that many teams are already over-worked, under-resourced, and looking to an uncertain future in which there may be a significant COVID surge. We recommend you follow the below steps in order to best understand capacity for your team.
How to Assess Your Team's Capacity
1) Assess your team’s bandwidth and any expectations regarding the extent of your participation. Consider asking yourself the following:
- What is my team’s current level of well-being? How well are we functioning?
- What is our current case load? Do we anticipate a surge?
- Do we have “shovel ready” resources that we can share, or do we anticipate needing to develop new resources?
- What are our motivations? What do we stand to gain and contribute by participating?
- For example, potential gains could include strengthening recognition of palliative care’s essential role in your organization, a seat at the table if your team’s wellness or lack thereof are systemic issues that need leadership attention; academic or scholarly interest for your own professional development
- What are the risks of getting involved? Diminished capacity to care for patients in need? Increased strain on already exhausted team members?
2) Research organizational emotional PPE efforts, which may already underway within your organization.
For instance, a growing number of hospitals and health systems are establishing Chief Wellness Officers, some of whom have budgets they can commit to high priority efforts. In other cases, it may be senior leadership, human resources, or alternate offices developing resources and programs. This can help you narrow down the translatable palliative care skills and resources your team has to support the organization’s efforts, without being duplicative or over-committing yourself or your team.
3) If your team decides it has the bandwidth to contribute to organizational efforts, align with those who are addressing emotional well-being.
If there is no centralized effort and your palliative care team (or an individual representative) wants to step in to fill the void, it is feasible to make an evidence-based case for why it should take on the role; however, please make sure to advocate for resources to support this work, be it dedicated time or salary supplement.
If you decide to proceed, please visit CAPC’s Organizational Wellness page for additional resources, which is in the Emotional PPE section of the COVID-19 Response Resources Hub. Furthermore, here are some additional external resources on emotional PPE to support your efforts:
- Sample Mount Sinai infographic and website
- National Academy of Medicine Action Collaborative on Clinician Well-Being and Resilience (link)
- Institute for Healthcare Improvement Psychological PPE materials (link)
- American Hospital Association (link)
- American Health Care Association/National Center for Assisted Living (link)
- New England Journal of Medicine, “Supporting Clinicians during COVID-19 and Beyond” (link)
If you are seeking additional support for COVID-19 response efforts, we encourage you to visit CAPC's Response Resources Hub, which has endless tools, technical assistance, and more – across numerous topics. Access is free for all health care professionals during the pandemic.
LEARN MORE



