“I Don’t See Color” Means You Don’t See Me
“All clients receive equal care, regardless of race.” “All patients are equally important to our team.” “We do not see color when it comes to care.”
These are just a few of the comments that CAPC received in response to a national survey sent out in late 2021, which aimed to collect information about improving the care of Black patients living with serious illness, and their families. (The survey is part of the Equitable Access to Quality Palliative Care for Black Patients project.)
Survey Responses
While we received hundreds of responses that will inform the future direction of CAPC’s health equity work—including interventions to improve cultural competence on palliative care teams, use of health care navigators in the community, and more—this wasn’t the case across the board.
We also received submissions that reinforced how much work the palliative care field still must do to move towards a more equitable health care system. A few responses were explicitly racist and therefore discarded. However, other responses, like those mentioned earlier, lived in the gray area of our evolving understanding of how to perceive, discuss, and act on issues of race. It was these that the CAPC staff and Equity Steering Committee spent much time processing.
On the surface, the earlier comments reflect the palliative care ethos of providing the highest-quality holistic, interdisciplinary care to any patient who enters the service. And it could be that the intention behind the idea of providing “equal” care was adhering to a process of conducting the same comprehensive assessment that would facilitate a customized, person-centered treatment plan that took into consideration factors such as race, ethnicity, impacts of systemic racism, social determinants of health (SDOH), etc. But taken together, the thematic nature of these comments started to read as “we treat all people the same.” This is a position that our field must move beyond.
Taken together, the thematic nature of these comments started to read as "we treat all people the same." This is a position that our field must move beyond.
Background on “Colorblind” Ideology
Paradigms for discussing race in the U.S. have evolved over time.
While it would be incorrect to say that our country has universally moved beyond the most racist and harmful approaches, it has been a few decades since “separate, but equal” has been the explicit curriculum in our children’s classrooms and beyond. (De facto segregation is still prevalent, but that is outside the scope of this blog.) Over the last few decades, many institutions have adopted a colorblind approach to discussing race; specifically, “the racial ideology that posits the best way to end discrimination is by treating individuals as equally as possible, without regard to race, culture, or ethnicity” (Williams, 2011). This is what many professionals currently working in and out of health care were taught in our formative years.
Colorblind ideology may have been necessary at one point in moving along the trajectory towards greater equity in our society, but it is an unacceptable place to stop.
Colorblind ideology may have been necessary at one point in moving along the trajectory towards greater equity in our society, but it is an unacceptable place to stop. Upon review, this ideology has been more accepted in white spaces where the opportunity to “not see race” is a point of privilege. It has been described as “dysconscious racism,” which invalidates the experience of Black, Latino, American Indian/Alaska Native (AIAN), Asian American/Pacific Islander (AAPI), and other populations, and perpetuates systemic racism. It misses the fact that all people do in fact see race, and that we develop racial biases starting from a very young age. Leaning into a colorblind mentality leaves proponents less equipped to recognize or engage in difficult conversations about race and racism. And it can create dangerous blind spots in health care delivery.
Yet, it has been difficult to move beyond the idea of racial colorblindness because most devotees are well-intentioned. Looking at palliative care specifically, many of us entered this field because of our own passion for alleviating suffering, regardless of a patient’s characteristics or circumstances. Palliative care is structured to meet the holistic needs of patients and families, which should make the field better equipped than most others to care for people of different races and ethnicities (including addressing the health-related consequences of systemic racism). Our field’s quality standards, the NCP Guidelines, have an entire domain titled “Cultural Aspects of Care.”
Palliative care is structured to meet the holistic needs of patients and families, which should make the field better equipped than most others to care for people of different races and ethnicities.
Unfortunately, recent publications on the prevalence and impact of racism in palliative care reveal that good intentions are insufficient. More broadly, there is a growing body of research demonstrating that generations of “colorblind care” have failed to address disparities ranging from overall health care access and outcomes to documented biases in electronic health records. Only with concerted and sustained attention to racial disparities—including interrogating our own implicit biases—can the field move forward to ensure that all patients living with serious illness have equitable access to high-quality palliative care.
The Importance of Unlearning Colorblindness
The popular image, included below, illustrates the difference between equality and equity. In the first panel, three people of different heights are standing on identical boxes to see a baseball game over a fence. The tallest person—who can see the game without assistance—towers over the fence. Meanwhile, the shortest person is still unable to clear the fence, even with the assistance of the box. This panel is labeled “Equality.” In the second panel, the shortest person has two boxes, while the tallest person has none. By rearranging the boxes based on each person’s needs, all are able to see the game over the fence. This is labeled “Equity.”
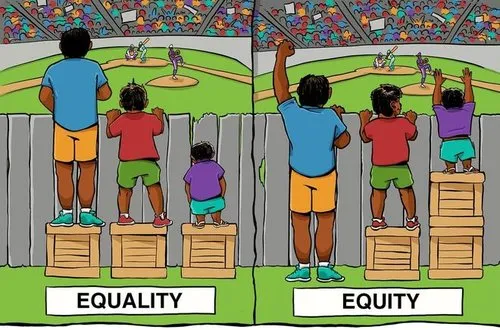
While this image has been critiqued as reductive (see the Center for Story-based Strategy’s “#4thBox”), it can be an effective starting point for this conversation. Colorblind ideology sits squarely in the first panel. It fails to recognize the different experiences, resources, challenges, and assets that diverse patients bring to every encounter. Clinicians who are reluctant to acknowledge these differences as they pertain to race and beyond miss critical opportunities to deliver patient-centered care. At a higher level, programs (like many of those seen in CAPC’s survey responses) miss opportunities to innovate, to create new initiatives that could address—rather than paper over—the disparities and inequities that permeate the health care system.
Clinicians who are reluctant to acknowledge these differences as they pertain to race and beyond miss critical opportunities to deliver patient-centered care.
Beyond the clinical and moral reasons to unlearn colorblind ideology, there are increasing policy imperatives to which all health care providers must respond. The Centers for Medicare and Medicaid Services (CMS) have named health equity as a pillar of their strategic priorities, including releasing a Framework for Health Equity and elevating “Advancing Health Equity” in its National Quality Strategy. Proposed rulemaking across CMS programs have included new proposals and requests for information regarding strategies to capture and address disparate care and outcomes for diverse beneficiaries. In other words, it is all but certain that CMS will begin to hold providers accountable for how they factor considerations such as social determinants of health, race, ethnicity, sexual orientation, gender identity, religion, etc., into a customized plan of care.
Equitable care is customized care that enables patients to achieve the best "quality of life possible based on their individual circumstances and goals."
Equitable care is customized care that enables patients to achieve the best quality of life possible based on their individual circumstances and goals. This may mean doing things differently for different patients. There are many reflection questions that clinicians can ask themselves if they feel committed to a colorblind ideology. One of the most powerful in our discussions was, if you find yourself wanting to say, “Our program treats everyone the same,” ask yourself, “Is that because all of our patients are the same?” In addition to reflection questions, several experts recommended storytelling as an effective strategy to help clinicians move beyond this mentality.
Storytelling
Storytelling in health care (an approach used within the field of narrative medicine) is a method by which clinicians elicit stories from their patients to recognize the meaning and significance of a diagnosis within the context of a person’s life story. Asking open-ended questions allows patients to tell of their experiences in their own words: “Why are we here today?”; “Can you tell me about your family?”; “How has this illness impacted you and your inner support circle?”
These types of questions allow patients to begin sharing their experiences in their own words. The clinician may go beyond by asking questions such as, “What is something you love doing?” or “What would you say is your greatest success?” While there are no perfect questions, the more you practice, the more you will find the ones that can elicit the most meaningful responses about who your patient is.
Consider the following example from my (Marisette Hasan's) personal experience:
The practice of storytelling played a significant role when my mother was diagnosed with metastatic colon cancer at age 48. Our care team was predominantly white, but as an African American RN, I was equipped to advocate for her. Prior to my involvement, no member of my mother’s care team knew her story, her family, or her faith traditions. My family took the time to help them get to know her, to understand that her fight would not be won solely by surgery and chemotherapy; rather, she would fight the good fight of “faith.” She believed that God was her healer, as many in her African American faith community believe.
By forging this deeper understanding, we were allowed to bring in her faith traditions to complement her medical care. We played gospel music from her culture in the room. We placed scriptural affirmations of healings on the wall and recited them as she took her medications. Her traditions were acknowledged and supported. If I had not been in a position to advocate for her, no one would have taken the time to ask her about her journey. Yet it was through storytelling that her care team was able to understand that faith and family were a part of her (our) roots, and made all the difference in her journey.
Yet it was through storytelling that her care team was able to understand that faith and family were a part of her (our) roots, and made all the difference in her journey.
This may seem basic—particularly for palliative care teams that, by definition, try to understand a patient’s circumstances—but the reality is that many of us are so busy that we do not ask these “extra” questions. Many patients want their providers to know that they are more than their medical history. And creating space to have these conversations is particularly important for Black patients, since the culture of health care remains predominantly white. Even though race (along with ethnicity, sexual orientation, gender identity, socioeconomic status, etc.) may not be the only component of patients’ stories, it often plays a significant role. Storytelling helps patients articulate where race fits in, and provides additional information that clinicians can use to individualize care. Beyond that, the act of being heard by the clinician can be healing.
Storytelling helps patients articulate where race fits in and provides additional information that clinicians can use to individualize care.
Beyond the individual clinical encounter, listening to stories can be instructive as programs seek to build new interventions to address disparities in health care. Cynthia Perrilliat of the AC Care Alliance explained that a “story listening” approach with spiritual leaders in the community helped identify systemic gaps. These stories helped inform what additional resources and supports were needed to support Black patients living with serious illness and their caregivers. Furthermore, storytelling goes beyond health care as an effective strategy for combatting racism in our broader society. Again, there is more information available on this topic than can be covered in one blog, but Dr. Camara Phyllis Jones’ lecture, “Telling Stories: Allegories on ‘Race’, Racism, and Anti-Racism,” and Lee Anne Bell’s Storytelling for Social Justice provide a wonderful starting point.
Conclusion
There is no shame in having embraced colorblind ideology. For many of us, this was part of our formative socialization, and the desire to see beyond color comes from a well-meaning place. However, intent is not impact. In an era in which many have declared racism as a public health crisis, every clinician must embrace a new way of navigating race and how that informs appropriate care for each patient. Respect for every patient includes “seeing their color” and affirming the impact of their culture on their personal story. Storytelling is an effective strategy to help move the field forward.
We must pursue cultural humility as a bridge to building authentic relationships with those we care for throughout the continuum of serious illness.
Furthermore, paradigms will continue to evolve. The road to cultural competence is never complete. We must remain open to growing in this area, even when it makes us feel uncomfortable. We must pursue cultural humility as a bridge to building authentic relationships with those we care for throughout the continuum of serious illness. One of the greatest challenges and opportunities we all face is how to accept corrections gracefully and then act on those corrections. CAPC will be adding to its health equity resources in the coming months.
Acknowledgements
The authors would like to acknowledge Katie Grogan, DMH, MA, and Cynthia Perrilliat, MPA for their contributions on the storytelling section of this blog.

