Introducing a New Administration to Serious Illness
Introduction
Living with serious illness is a human issue that transcends politics and party affiliation. As an organization dedicated to improving quality of life for people with serious illness, The Center to Advance Palliative Care’s (CAPC) responsibility is to educate policymakers and other key stakeholders on the issues facing our population, along with policy changes needed for its benefit. The installment of a New Administration presents a crucial opportunity to educate a brand-new audience on the challenges of living with serious illness and the barriers in caring for these patients and their families/caregivers.
Therefore, CAPC was pleased to participate in an initiative led by The Pew Charitable Trusts to develop a consensus-based memo for policy leaders. This initiative brought together representatives from policy advocacy organizations, health associations, consumer coalitions, the health insurance industry, and hospice organizations, to “jointly identify policy recommendations to the next administration and Congressional members to improve the quality of, and access to, palliative care and end-of-life care.” Developing these recommendations was a truly collaborative effort; it resulted in a document that highlights a sampling of policy priorities from several organizations working in this space and can be used to support future advocacy. Just as importantly, however, the process demonstrated an overwhelming commitment by our organizations to improving quality of life for the vulnerable people we serve and their families/caregivers.
The Work of Coming Together
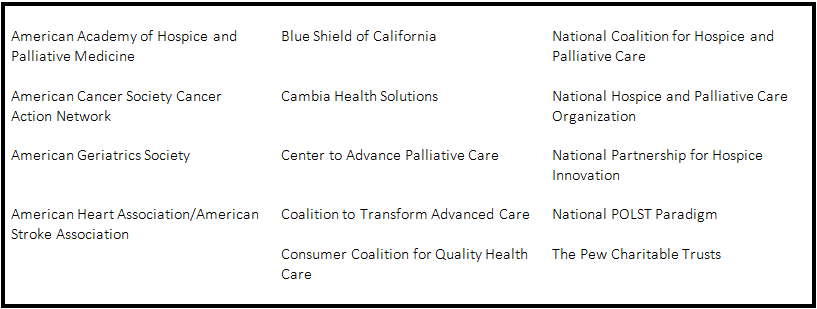
Pew spent several months prior to the first meeting identifying a small group of experts and advocates in the field to participate in this process. Ultimately, the following organizations participated in the development of the memo and signed on, although the final document benefited from the contributions of several additional organizations throughout the process:
Once participants were selected, the process of bringing people together, identifying target areas, focusing priorities, and drafting the recommendations took approximately six months. Activities included:
- pre-workgroup interviews to gather individual organization’s opinions on the policy challenges and opportunities and identify any potential inter-organizational differences and concerns;
- five in-person meetings held in Washington, DC, including two meetings to agree on the most pressing policy categories;
- telephonic subcommittee work, in which smaller groups developed specific recommendations within each broad category; and
- numerous phone meetings and emails to write, refine, and iterate the recommendations.
Along with differing population perspectives (i.e., geriatrics, cancer, heart disease, pediatric illness), the group was able to ensure that each of our priorities were represented while keeping the document coherent enough to make the recommendations compelling. As discussed in a previous Palliative in Practice post, there remains much variability in how organizations working in our field describe care for people with serious illness. With that tension in mind, the group worked through several different topics to reach consensus on the most appropriate language and/or reference point; for example:
- using person-centered vs. patient-centered
- defining palliative care, serious illness, hospice, and advance care planning (ACP)
- focusing on issues specific to our population vs. including relevant broader issues that are already being addressed by other advocacy organizations (e.g., health information interoperability)
It is also worth noting that the process began in August 2016 – roughly two and a half months before the election. This meant that we had to develop recommendations that would resonate with policy leaders regardless of their party affiliation.
The Recommendations
The group made recommendations in four categories:
Building a Robust Workforce Through Education and Training. These recommendations call for increased education and training opportunities for those caring for patients with serious illness. Areas of focus include health professions education and training programs, and graduate medical education.
Promoting Measures and Care Models that Improve Quality. These recommendations call for an investment in quality measures that capture patients’ values, care goals, and treatment preferences over time and establishing thoughtful mechanisms for accountability. They also urge the New Administration and Congress to extend and improve innovative models of care that expand use of palliative care, refine and expand models – like the Medicare Care Choices Model – that incorporate concurrent care, and adopt models of public-private partnerships that increase access to palliative care and hospice for veterans.
Supporting Research to Strengthen Palliative Care and End-of-Life Care Practice. These recommendations call for increased investment in research and strategizing by the National Institutes of Health (NIH) to expand the knowledge base to strengthen clinical practice and health care delivery, and yield meaningful evidence to improve the quality of care and quality of life for patients with serious illness.
Improving Health Information Technology to Honor Patients’ Preferences. These recommendations reaffirm not only the importance of advance care planning conversations between patients and clinicians, but also the need to include standards for certified electronic health record technology so that ACP documentation is easily accessible.
Click this link to read the PDF of the full memo.
Next Steps
Pew submitted the letter to Representative Tom Price, the Secretary of Health and Human Services, and to Representative David Shulkin, the Secretary of the U.S. Department of Veterans Affairs, on 2/22/2017. Between confirmation hearings, Affordable Care Act repeal-replace discussions, and various executive orders, the truth is that this memo is unlikely to make an impact in the early days of the New Administration. However, having gone on record voicing the most pressing policy issues for seriously ill patients, our organizations have a new platform for future advocacy. Several plan to bring the memo with them to Capitol Hill for upcoming meetings with members of Congress and heads of various agencies. The full workgroup is also considering planning a webinar to describe the recommendations in fuller detail, as well as a possible Hill briefing in early spring once the transition work is complete.
In the meantime, we are looking for additional organizations that would like to endorse the memo. If your organization is interested in strengthening the voice on these recommendations, please contact [email protected].
