Bringing Home-Based Palliative Care to Scale with Effective Program Design
This is part one of a two-part blog series in which Jeanne shares highlights from CAPC’s home-based palliative care interview series. Elements of program design are discussed in detail, including patients served, services offered, and the interdisciplinary team.

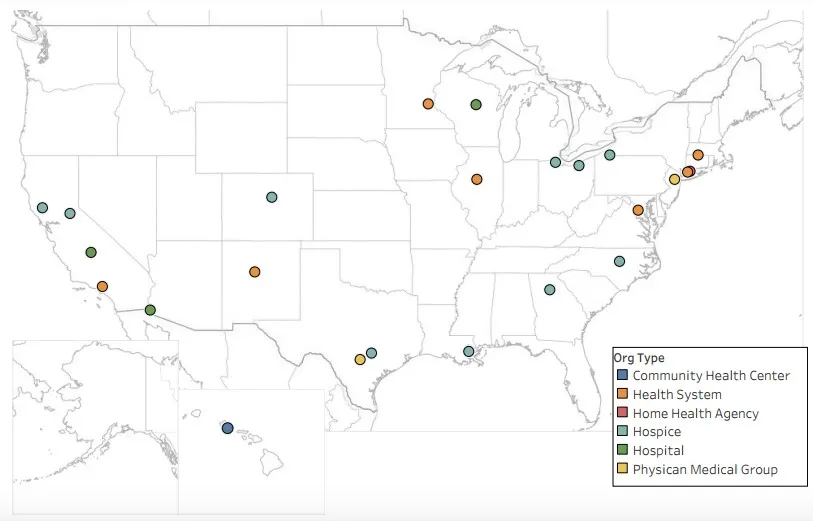
Access to home-based palliative care (HBPC) is vexingly limited. Thanks to a grant from the Cambia Health Foundation, CAPC explored how to reliably assure availability of HBPC. To get answers, CAPC surveyed and interviewed leaders of rank-and-file HBPC programs–large and small, urban and rural from across the country–to identify barriers to care delivery and discuss solutions. We’re sharing interview highlights below.
Appropriate Referrals Depend on Consistent Criteria
Challenges
- Lack of a shared understanding of palliative care and standardized patient eligibility criteria pose barriers to accurately identifying appropriate patients, and require ongoing partner/referrer education.
- Vague or overly broad eligibility criteria lead to confusion. The result: late or inappropriate referrals; inability to meet needs of referrers, patients, and families; and threats to credibility when programs fail to meet expectations.
- Programs want to “take all comers” versus having more narrowly defined eligibility criteria that ensure the feasibility of well-managed, well-delivered care.
Tips from the Field
- Clearly define palliative care as an added layer of support to reduce referrers’ fear that the HBPC program will interrupt—or take over—existing clinician/patient relationships.
- Use a stakeholder needs assessment to define program eligibility criteria; assure criteria address the program’s goals and its target population.
- Continuous stakeholder education about palliative care and eligibility criteria increases the likelihood of appropriate referrals.
- Start with narrow criteria: pilot the eligibility criteria before scaling the program and take program capacity into account.
- Adhere to eligibility criteria when identifying and accepting patients; then, continuously monitor and reassess.
Continuous stakeholder education about palliative care and eligibility criteria increases the likelihood of appropriate referrals.
How CAPC Can Help
- Take the community-based palliative care needs assessment toolkit and corresponding CE course.
- Sample HBPC program brochures for patients and referrers.
Barriers to Identifying High-Need Patients
Challenges
- HBPC programs may not have the expertise or the access needed to use claims and clinical data to identify high-need patients, or to demonstrate that services reduce the cost of care for these patients.
- Triggers can lead to earlier palliative care referrals but require an integrated data system which is often not available to programs: lack of EHR interoperability is a challenge.
Tips from the Field
- Using clinical and claims data to identify appropriate patients increases the likelihood of reaching patients most in need, and shows the greatest financial impact.
- Automated triggers are particularly necessary if the program or organization is taking financial risk.
- Trigger parameters must align with the shared vision and needs of the “risk takers” (payers, ACOs, or provider organizations).
- Cultivate and nurture relationships with referrers, even when using automated triggers.
How CAPC Can Help
Assuring Interdisciplinary Holistic Care for Seriously Ill Patients
Challenges
- Care provided in the home is complex, time-consuming, and must encompass attention to patients’ medical, psychosocial, spiritual, and environmental issues.
- Adequately addressing patients’ psychosocial needs is the top service challenge, particularly when programs cannot afford to include adequate social work and spiritual care due to lack of reimbursement.
- Programs that fail to offer comprehensive services will not meet patient needs or achieve necessary outcomes or sustainability.
Tips from the Field
- Design the service package with patient need as the focus. Let the National Consensus Project (NCP) Clinical Practice Guidelines for Quality Palliative Care be your guide.
- Use eligibility criteria to develop a protocol to stratify patients by level of need; customize service packages to meet each level as a strategy to deliver high-quality, cost-effective services.
- Leverage telemedicine as an effective approach to delivering interdisciplinary care.
- Establish a network of community providers/partners to serve as referral points for meeting patients’ needs in the home.
- Without clarity on your program’s service package and model of clinical responsibility it is impossible to define the appropriate team composition.
How CAPC Can Help
- Utilize CAPC tools for estimating program costs and staff capacity.
- Review CAPC's telehealth resources, part of the Designing a Home Based Palliative Care Program toolkit.
Staffing: Consider the Complexities
Challenges
- Workforce shortages are rampant for specialty-trained staff in all clinical disciplines delivering HBPC.
- Program quality is compromised by challenges with staff recruitment, retention, and compensation, as well as team composition, staffing ratios, and training.
- Programs struggle to financially support a full interdisciplinary team; sharing staff with other programs or organizations can help, but requires additional training and can result in fragmented care.
- Home settings must be staffed by experienced individuals who can balance autonomy with team playing, and are comfortable in an unpredictable and isolating environment.
- Finding and keeping skilled, experienced, “right fit” staff is difficult, particularly in a marketplace where compensation packages for HBPC staff are rarely competitive with other health care organizations.
Tips from the Field
- An individual’s comfort working in the home environment is the most important attribute to consider when recruiting. Also consider capacity to adjust in real time to challenging or unpredictable occurrences and comfort with some degree of autonomy.
- Involve current staff in interviews; use shadowing during the hiring process to assess a recruit’s comfort working in the home environment.
- Staff cannot “float” interchangeably across HBPC, hospice, and home health programs without adequate palliative care training and consensus on organizational boundaries regarding time allocation.
- Implement a robust orientation process, provide mentoring during onboarding, and clearly delineate staff roles and responsibilities.
- Programs can increase staff capacity through a well-developed volunteer program.
An individual’s comfort working in the home environment is the most important attribute to consider when recruiting.
How CAPC Can Help
- Building and Supporting Effective Palliative Care Teams, which includes job descriptions, service agreements, and more!
- Use the Designing a Home-Based Palliative Care Program toolkit, specifically the 'Tools for the Home Visit'.
- View all Online Training Courses for Clinicians, where you can find the full course catalog, with information about continuing education credits and MOC points.
- Learn Quick Tips for team effectiveness, within the Building and Supporting Effective Palliative Care Teams toolkit.
Addressing Retention, Resiliency, and Burnout
Challenges
- Addressing turnover and burnout is a perpetual challenge that drains resources.
- Inconsistent salary structures within the field across care settings contribute to staff turnover, particularly for nurses.
- Insufficient endorsement by leadership of the importance of allocating time for program design, strategic planning, and leadership development are demoralizing for staff.
Tips from the Field
- Reduce opportunities for burnout: assure expectations stated in the job description are in sync with the actual work; align workload with staff volume; provide sufficient support staff to achieve clinical efficiency; invest time and resources in team wellness; offer flex time and staff rotation.
- Combat the stress of working alone in the home environment with regular team huddles via teleconferencing and weekly face-to-face meetings.
- Support the autonomy/decision-making power of clinical staff who work alone in the home.
- Address resiliency: debrief at team meetings; offer opportunities to reflect; integrate self-care practices; and, systematically monitor staff resiliency through quality-of-life surveys.
How CAPC Can Help
- Review telehealth resources, part of the Designing a Home Based Palliative Care Program toolkit.
- Review Quick Tips for “Improving Team Effectiveness: Team Health and Resilience”.
Additional Resources
- Learn how to successfully design an HBPC program by attending CAPC’s Pre-Seminar Boot Camp: Designing Palliative Care Programs in Community Settings on November 13, 2019. Save the date!
- For HBPC program profiles and in-depth information on program startups, please reference CAPC’s Palliative Care in the Home: A Guide to Program Design.
- Read part two for perspectives on HBPC quality, financial health, and program sustainability.
