4 Ways You Can Take Action with CAPC’s New Serious Illness Scorecard
Over the last two decades, there has been tremendous growth in the field of palliative care, with over 80 percent of U.S. hospitals with 50 or more beds reporting a palliative care program in 2020 (up from 24.5 percent in 2000). More recent years have brought a surge of state and federal activity, palliative skills training, and caregiver supports, all driving better care of people living with serious illness. This evolving landscape requires a new way of describing our country’s capacity to provide the best care for people with serious illness—going beyond hospital-based palliative care to incorporate community-based palliative care, clinical training, private payer initiatives, and advocacy structures.
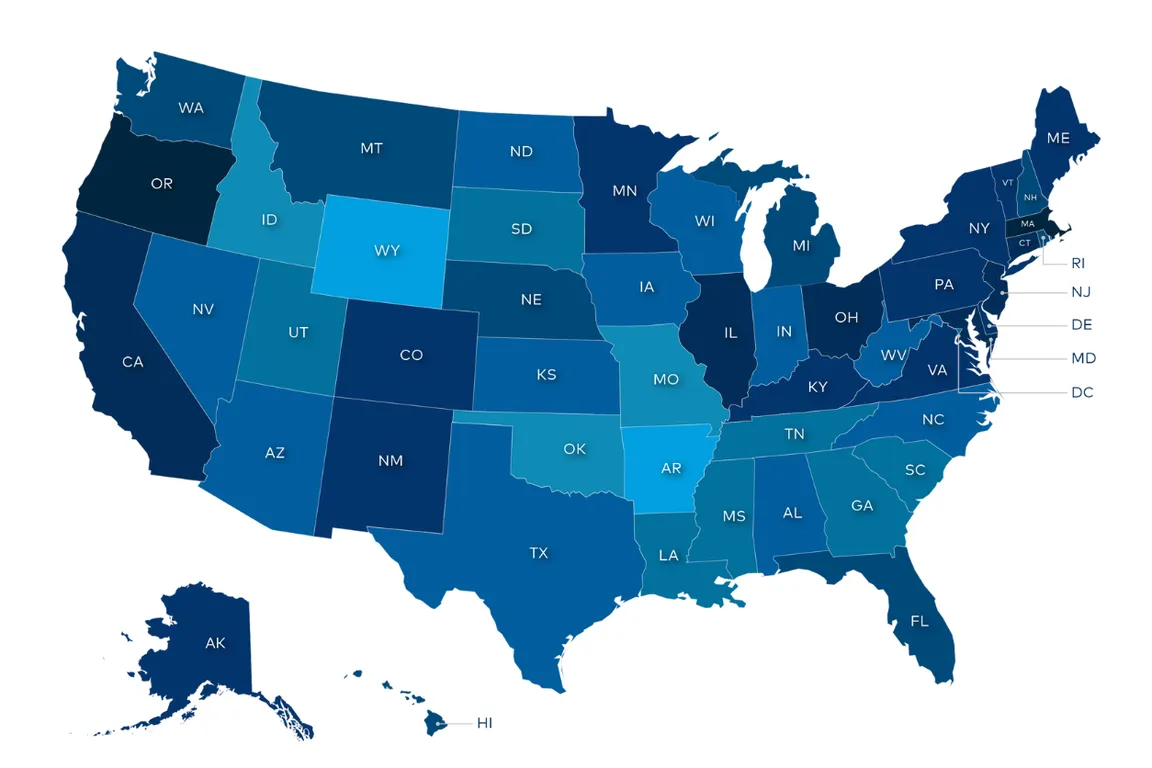
Enter the Serious Illness Scorecard (“Scorecard”). This new resource assesses the current state of support for people with serious illness nationwide. Each state is given a rating based on ten items across five domains. This rating—accompanied by newly expanded, individual state reports—provides palliative care leaders with a road map for assessing their state’s status, comparisons to other states across the country, and recommendations to improve palliative care access in their state or region.
The Scorecard Builds on the State-by-State Report Card™
Prior to the launch of the Scorecard, CAPC and the National Palliative Care Research Center (NPCRC) published four editions of “America’s Care of Serious Illness: the State by State Report Card” between 2006 and 2019. It was a successful tool for increasing awareness of palliative care, tracking the growth of the field, and encouraging policymakers to take action.
Since its launch, the number of states with a palliative care team in at least 80 percent of its hospitals with more than 50 beds increased from three to twenty-one in 2019. In the 2019 Report Card, three quarters of states had palliative care in more than 60 percent of their larger hospitals. The launch of each Report Card had an incredible impact, educating key parties on what palliative care is and helping to grow federal lawmaker support for the Palliative Care and Hospice Education and Training Act (PCHETA), which passed in the House of Representatives in two consecutive legislative sessions.
Happily, the palliative care field has now grown well beyond the four walls of the hospital, and palliative approaches to care delivery are exploding across all health care settings. CAPC has created the new Serious Illness Scorecard to reflect the multitude of efforts to improve care for this population.
How the States Were Scored
The new Scorecard considers ten variables that describe how well a state is equipped to meet the needs of people living with serious illness and their caregivers. These include the domains listed in Figure 2, below.
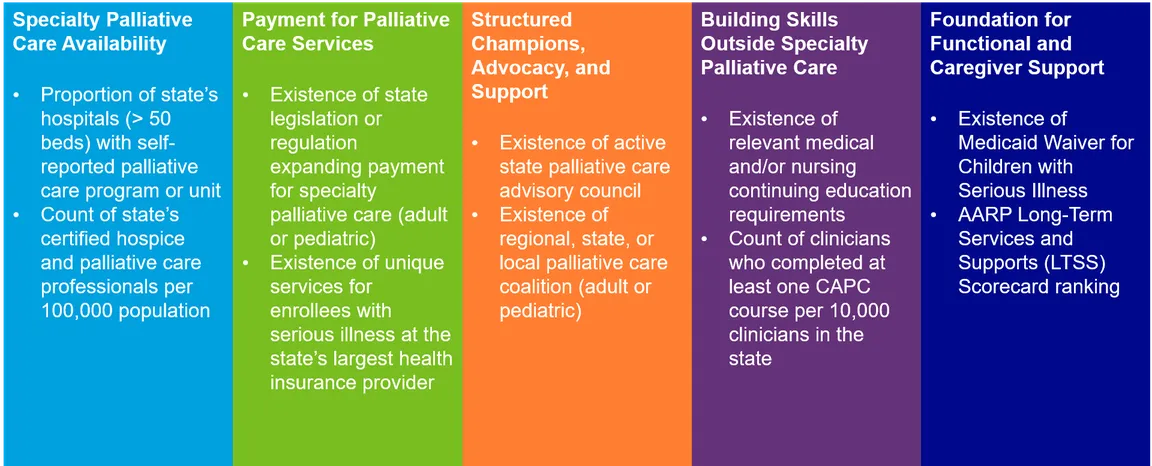
The Scorecard combines information on availability of specialty palliative care with other key factors that impact the care of people living with serious illness. In so doing, the Scorecard provides a more nuanced portrait of where states stand and helps champions better identify opportunities for continued improvement.
"In this inaugural version of the Scorecard, no state has achieved five stars; this means that champions can identify at least one goal to work towards in their state."
How to Take Action Using the Scorecard
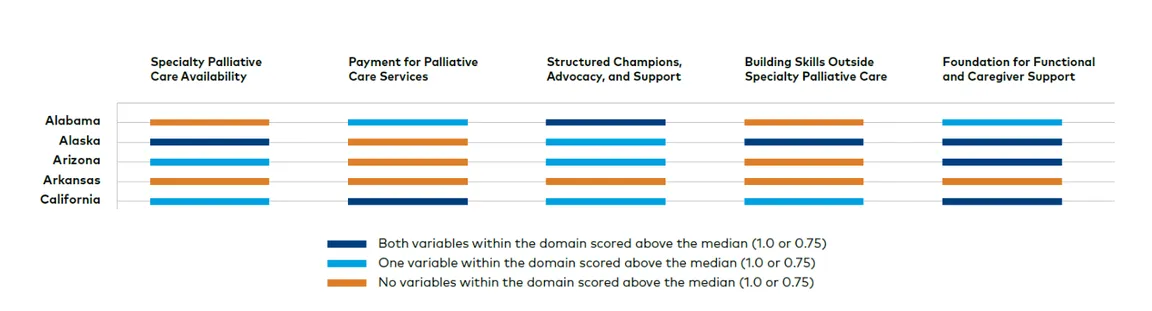
The new methodology uses the ten variables above to calculate a score between 0 and 5. In this inaugural version of the Scorecard, no state has achieved five stars; this means that champions can identify at least one goal to work towards in their state. To help you target areas for improvement, we have created the following resources:
● The "State Performance by Domain" table, where you can quickly see which domain(s) need attention in your state (sample image below);
● A complete state rating appendix table, which provides more detail on how your state scored in each factor; and
● New individual state reports, which go into greater depth on some of the Scorecard factors, as well as other indicators that impact quality of life for people facing serious illness.
● A social media kit, which includes shareable posts and images of your state's rating, in-depth information about access to palliative care in your state, and recommendations for improvement.
Depending on the gaps in your state, potential actions can occur at the organizational, professional association, regulatory, or legislative levels. Both the Scorecard website and the downloadable state reports include high-impact recommendations for action; you should select the recommendation(s) that best corresponds to the identified gaps and that you judge to be feasible, given the local political climate. Some examples of how to take action—including a few that may directly improve your state’s score--are as follows.
NOTE: It is critical that any policy action is taken as part of, or in concert with, established palliative care or serious illness leadership organization(s) in your state! Your individual state report includes a list of any active entities that we could find at the time of publication. If you are aware of any omissions, please contact [email protected].
1. Building Skills Outside Specialty Palliative Care
While it is essential to continue growing the specialty palliative care workforce, there will never be enough specialists to meet the needs of all people living with serious illness—and all clinicians caring for people with serious illness can benefit from basic palliative care skills. Therefore, it is critical to educate all clinicians on how to: 1. Communicate effectively with their patients; 2. Manage pain and other symptoms within their scope of practice; 3. Support caregivers; and 4. Refer to specialty palliative care when appropriate.
One of the best places to start working towards this goal is at the organizational level. For instance, many clinicians do not know they have access to CAPC resources. You can encourage colleagues to check whether their organizations are members, and if so, there are several resources available to help palliative care champions get the most out of CAPC's clinical education resources. Palliative care education initiatives can ensure a common base of knowledge in essential skills, and enable clinicians to work more collaboratively to improve care for seriously ill patients.
2. Programmatic Expansion
Historically, palliative care leaders used the report card to advocate for palliative care service expansions into “sibling” hospitals. Indeed, hospital-based palliative care remains essential to high-quality care for people with serious illness, and relying on comparisons to other states via the Scorecard can motivate health system leaders to expand specialty palliative care into additional acute facilities. Note this may include academic medical centers and tertiary hospitals providing care via telehealth to other hospitals.
3. Growing the Base for State Palliative Care Champions
Multi-entity coalitions that focus on addressing the needs of people living with serious illness have been essential in advancing improvements through public awareness, education, and policy initiatives. Successful examples include (but are not limited to) the Coalition for Compassionate Care of California, the Goals of Care Coalition of New Jersey, and the Washington Serious Illness Care Coalition. The individual state reports can help identify if you have a relevant entity in your state that you can join. If such a coalition does not exist in your state, one of the ways in which you can improve your score is to establish one. The Coalition to Transform Advanced Care (C-TAC) developed an in-depth resource on community engagement, which walks leaders step-by-step through the work of building a coalition. State home health and hospice associations may be a good place to start.
4. Advancing State-Level Policy to Support Palliative Care
Several variables in the Scorecard require some level of direct policymaking. For instance, over half of states have a legislatively established advisory council or similar body that leads awareness or advocacy activities. Still, many states have either not taken this action or the councils have sunsetted or gone dormant. If your state does not have a council or you would like to explore options to revitalize an existing one, reaching out to your state chapter of the American Cancer Society Cancer Action Network (ACS CAN, click on “My State ↘” near the top right) is a good place to start.
Beyond that, many state officials, including legislators, government agency staff, medical and nursing boards, and others are interested in learning about opportunities to improve quality of life and the value of health care for their residents. Working through any councils, coalitions, or associations in your state, use the Scorecard and your individual report to identify potential “asks”—e.g., adding continuing education requirements on palliative care or relevant topics; advancing Medicaid payment for palliative care; or codifying specific additional services into Medicaid waivers for children living with serious illness. Use the Scorecard and your individual state report in meetings to frame the needs in your state. In addition to highlighting your state’s rating, review how your state compares to others in your region – in this case, a little healthy competition can be helpful!
Message Discipline Remains Imperative
Many of the actions recommended in this blog and the Scorecard require engaging with audiences outside of the palliative care field, i.e., audiences that still may not understand what palliative care is, who should receive it, or how it can improve quality of life for all people living with serious illness. CAPC offers free and open resources, including a recent webinar on how to message palliative care effectively.
Conclusion
The field of palliative care has come a long way, driving the need to create new resources to support continued transformation in the care of people living with serious illness. The Serious Illness Scorecard tells a comprehensive story about state-level capacity today and provides a roadmap of actions that state champions can take to improve future care.
"The Serious Illness Scorecard tells a comprehensive story about state-level capacity today and provides a roadmap of actions that state champions can take to improve future care."
Do you have additional suggestions or questions about how to leverage the Serious Illness Scorecard or individual state reports? Email [email protected] to share your thoughts!

Be the first to read articles from the field (and beyond), access new resources, and register for upcoming events.
SubscribeEdited by Melissa Baron. Clinical review by Andrew Esch, MD, MBA.


