Want to Strengthen Connection Within Your Palliative Care Team? Try Narrative Medicine

We are two professionals with different backgrounds, living on opposite coasts, who got to know one another as classmates in a narrative medicine certification program through Columbia University.
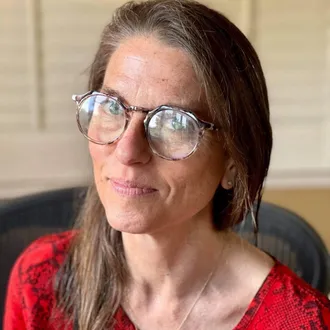
One of us, Eve Makoff, MD, MA, is a palliative care physician and writer who serves as Regional Medical Director for AltaMed Health Services, a government-funded community health network, providing wrap-around care to low-income elderly patients in Los Angeles, California. Eve is pursuing a master’s degree in narrative medicine at the USC Keck School of Medicine. The other is Katie Grogan, DMH, MA, Associate Director of Clinical Education at the Center to Advance Palliative Care (CAPC), where she works with field leaders to develop interdisciplinary clinical training curricula. Katie previously led a medical ethics and humanities program for students and trainees at NYU Grossman School of Medicine.
What is narrative medicine?
If you are unfamiliar with narrative medicine, it is a growing interdisciplinary field that fortifies clinicians with skills drawn from the arts, humanities, and social sciences. Chief among these skills is the ability identify, absorb, interpret, and respond to the stories that unfold in the context of illness. Expanding one’s narrative competence can deepen therapeutic partnerships with patients and strengthen connections within clinical teams. We are eager to share more about it, as it has had a tremendous impact on both of our professional and personal lives, and we think it could positively impact you and your teams.
Narrative medicine a growing interdisciplinary field that fortifies clinicians with skills drawn from the arts, humanities, and social sciences.
We recently interviewed one another via Zoom to collaborate on this blog post. We discussed what drew each of us to narrative medicine, how it connects with palliative care, and what benefits it may offer interdisciplinary teams. We close by sharing some ways you can incorporate narrative medicine into your practice.
Katie Grogan (KG): As a palliative care clinician, how did you find your way to narrative medicine?
Eve Makoff (EM): It started with racial health justice. I joined an online group of women physicians focused on social justice called SOAR (Support. Organize. Advocate. Reclaim.). In the midst of learning about racism in medicine, I had a very impactful patient encounter. I was working as a palliative care doctor in a cancer center, and a patient, who was a Black woman, was referred to me for anxiety by her oncology team. What she said to me was, “I’m not anxious. My cancer is growing, and nobody believes me, so they won’t order a CAT scan.” And I realized they were just not listening to her. She was not being heard about what she knew about her own body. As I got to know her, she shared many stories with me—both inside and outside of health care—where people had doubted what she told them about herself.
It connected everything I was interested in and offered a way to explore how individual patient stories intersect with broader systems and structures.
I was moved by her experience and wrote a case report on racial trauma, published in the Journal of Palliative Medicine. I sent it to one of my undergraduate English professors, and she asked if I’d ever heard of narrative medicine. I looked into it, and my mind was blown. It connected everything I was interested in and offered a way to explore how individual patient stories intersect with broader systems and structures. I knew I needed to do this.
EM: I have the same question for you, though in reverse. How did you find your way from narrative medicine to palliative care?
KG: Like you, I was first introduced to narrative medicine by an English professor. She had cared for patients with serious illness as a nurse, before becoming an academic. I took one course with her, and that was it—I knew I wanted to keep studying narrative medicine. When I finished my doctorate in medical humanities, I started co-directing and teaching in a medical ethics and humanities program at NYU. I was on the lookout for my people—folks who were interested in the centrality of storytelling in medicine and the lived experience of illness, not just the biological process of disease in abstraction of its meaning within the context of one’s life. I found that orientation in the palliative care faculty and trainees at my organization, and, conveniently, some of them had already heard of narrative medicine!
We then offered various courses that engaged narrative medicine techniques and had a lot of participation from folks interested or involved in serious illness care. We often called on palliative care faculty for teaching, and student mentorship in the various ethics and humanities programs.
KG: Tell me about the narrative medicine workshops you’ve been facilitating lately.
EM: In a basic workshop, we come together in a small group—fifteen to twenty max—and either read a poem or short story, look at a work of visual art or a film clip, or listen to a piece of music. Often, they’re not blatantly about serious illness, but they evoke relevant themes like finding strength amidst adversity, navigating ambiguity, or contemplating identity. We do a collaborative close reading as a group, and then we write to a prompt, inspired by something that arises from the text. For example, if we’re discussing a painting that depicts a storm, the prompt might be, “Write about a storm.” It’s deliberately very open-ended, so participants can go anywhere with it—a literal storm, turmoil in a relationship, a flood of emotions after a patient encounter. Then we share what we’ve written and respond to each other’s writing. It’s not about the quality of the writing; it’s about practicing reflection and self-expression. For instance, "What did the prompt evoke for you?” “Where did it take you?”
It’s not about the quality of the writing; it’s about practicing reflection and self-expression.
Recently, I’ve been doing a series of workshops with a group of family medicine residents within my organization. Their patients are mostly low-income, and many have past traumas. What I’ve found among the residents is an incredible need for them to talk about what they’re feeling as they go through their training. Narrative medicine has offered the residents a unique way to delve into big, overwhelming questions. This may include how to create their identities as doctors, and how to process challenging experiences or difficult emotions as they care for patients.
In my workshops with palliative care teams at various institutions, the clinicians are already used to the language of vulnerability. They are comfortable with uncertainty, so it’s less about helping them engage emotionally and more about giving them this opportunity for robust team-building.
EM: Are you using your narrative medicine training in your work at CAPC?
KG: Absolutely, palliative care and narrative medicine share many common goals: making patient care better and more equitable; centering the voices of patients and families; relieving suffering; and bearing witness. I think the distressing questions that come up in the context of a serious illness diagnosis—“Will I suffer from this?” “What gives my life meaning?” “How do I make sense of what’s happening?”—can be seen as narrative in nature. They’re about someone’s life story and how the plot and timeline are going to unfold. And there are also narratives in medicine around pain and illness that historically have been harmful to both patients and clinicians. CAPC is in a prime position to help change those stories and advance new ones.
Narrative medicine is inherently interdisciplinary, so it’s a helpful approach to creating learning experiences intended for everyone from nurses to social workers to chaplains to doctors.
Bringing this narrative lens to bear can be very impactful. I try to use it in helping to develop CAPC’s clinical training curricula, attending to how everything from our technical and figurative language to our illustrations and graphics advance a particular narrative about what palliative care is, who needs it, and how to provide it. Narrative medicine is inherently interdisciplinary, so it’s a helpful approach to creating learning experiences intended for everyone from nurses to social workers to chaplains to doctors. But in a more applied sense, narrative medicine workshops would be incredibly effective for all folks training in palliative care and within interdisciplinary palliative care teams. This is because there are so many shared concepts and values between the two fields, and because narrative medicine stands to support team members who have experienced so much grief and isolation throughout the pandemic.
KG: How have you seen narrative medicine fortify palliative care teams?
EM: The value is really in self-nourishment. Even with debriefings, palliative care clinicians don’t always get the time to digest their experiences and try to heal. Especially during COVID, palliative care teams have been so busy attending to others, and narrative medicine provides an opportunity for self-expression and self-reflection. These workshops cultivate an openness and a vulnerability that I believe coheres teams and allows people to trust and rely on each other more. The bond with the group, after doing this collaborative reading and sharing, is this sort of magical thing. You feel closer to the people you work with and can better support one another.
The bond with the group, after doing this collaborative reading and sharing, is this sort of magical thing.
Narrative medicine workshops are also useful for fostering diversity and inclusion. In narrative medicine, we’re trained to hold space for divergent perspectives and interpretations and to choose texts that showcase a diversity of voices. This lets us start to unpack biases in medicine. Doctors have been taught to speak and write about patients in certain ways. But what kind of narrative does the chart really tell? What kinds of stories do we perpetuate with language like “non-compliant” and “frequent flyer”? Narrative medicine helps us get into and out of complex issues in medicine together. It’s the best team-building activity that I’ve come across.
Consider incorporating narrative medicine with your team
Narrative medicine can positively influence everything from professional development to burnout to social justice. There have specifically been recent calls for the inclusion of narrative medicine in palliative care education and training. Narrative medicine is a highly accessible modality with tremendous benefits to individual clinicians and team wellbeing. Engaging in this work allows participants to sustain multiple dimensions of their identities, connects groups through fostering vulnerability and mutual purpose, and provides a unique tool for navigating the challenging work of listening and responding to the stories shared in the context of serious illness care.
Narrative medicine is a highly accessible modality with tremendous benefits to individual clinicians and team wellbeing.
How to start
If you would like to bring narrative medicine to your palliative care team, there are various approaches you can take. Many academic health centers now offer some form of narrative medicine, so you might start by contacting those faculty about facilitating workshops for your clinicians. Additionally, there are multiple narrative medicine certification and master’s programs across the US. Two are linked below, but there are several others. See what programs are near you, and reach out about hiring their graduates to lead workshops with your team. These can be delivered effectively both in-person and virtually. Finally, you might like to pursue narrative medicine training yourself! You can connect with others and learn to apply the principles and practice of narrative medicine through the following steps:
- Attend free virtual narrative medicine group sessions or Narrative Medicine Rounds
- Explore workshops with Columbia University or the Northwest Narrative Medicine Collaborative
- Learn about various certificates and programs in narrative medicine

Be the first to read articles from the field (and beyond), access new resources, and register for upcoming events.
SubscribeEdited by Melissa Baron. Clinical review by Andrew Esch, MD, MBA.