Comparing the Value of High vs. Low Touch In-Home PC Models
Research Objectives
In-home palliative care (IHPC) has emerged as a highly-accessible health care service with the potential to manage patients’ symptoms and keep them out of the hospital. The purpose of this study is to characterize the value, in terms of both quality and financial benefits, that two upstream IHPC models offer to seriously chronically ill patients.
Methods
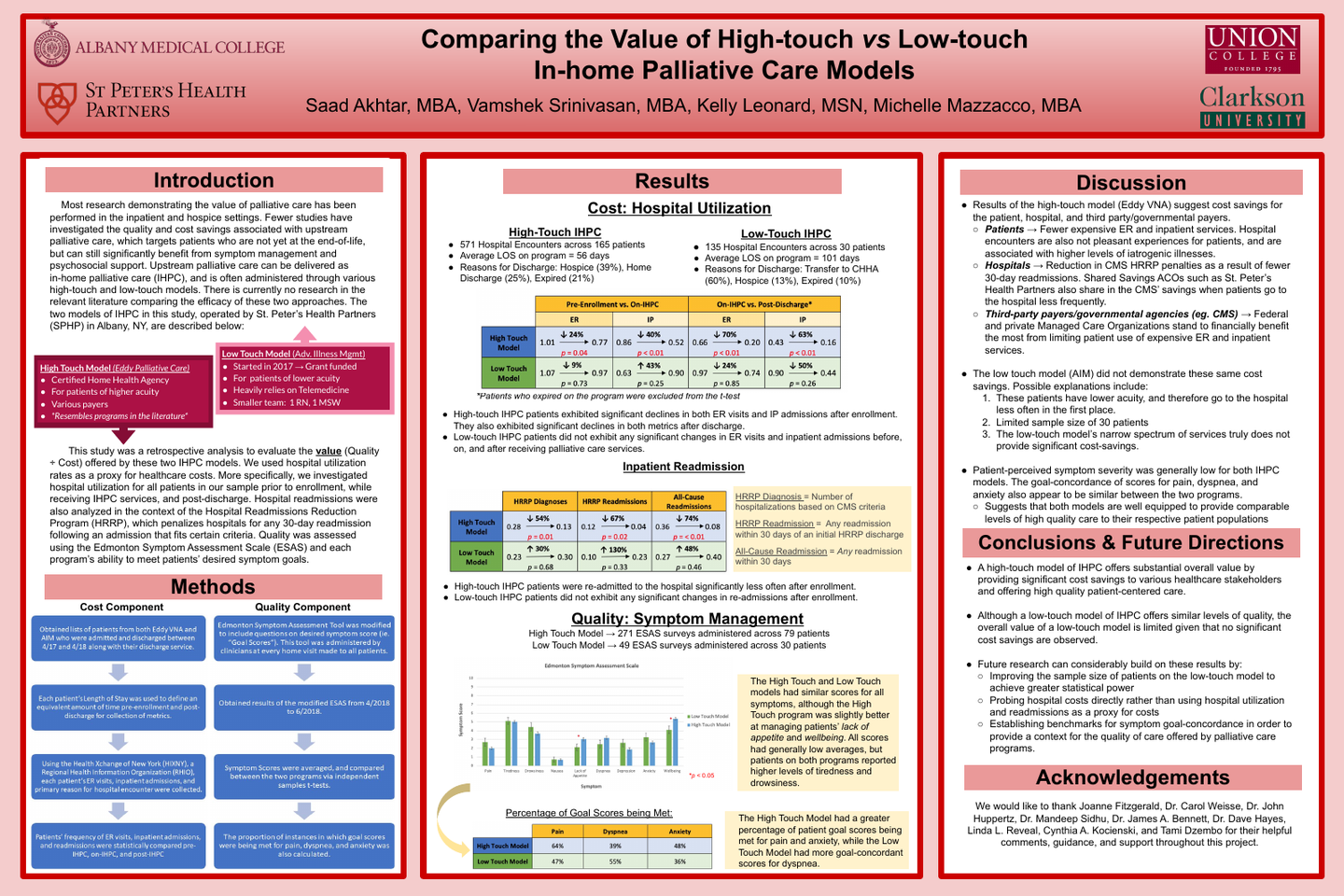
This study was a comparative retrospective analysis of patients on two IHPC programs offered in the Capital District of upstate New York: A High-Touch and a Low-Touch IHPC program. The high-touch model offers a wide spectrum of palliative care services and is operated through a Certified Home Health Agency that requires patients to have a skilled nursing need. The low-touch model offers palliative care through telemedicine and infrequent home visits, and is targeted at lower acuity patients who do not have a skilled nursing need. To assess the cost savings associated with each program, emergency room (ER) visits, inpatient admissions, and 30-day readmissions were evaluated for patients before, during, and after receiving IHPC. A Regional Health Information Organization was used to capture patient visits to any hospital in the region. The quality of care offered by both programs was investigated using a modified Edmonton Symptom Assessment Scale (ESAS) to assess patient-perceived symptom severity and goal scores.
Results
After enrolling on the high-touch IHPC program, 156 patients had 24% fewer ER visits (p = 0.04), 40% fewer inpatient admissions (p < 0.01), and 39% fewer all-cause readmissions (p = 0.04). Post-discharge from the high-touch IHPC program, patients had 74% fewer ER visits (p < 0.01), 69% fewer inpatient admissions (p < 0.01), but no significant change in 30-Day Readmissions (p > 0.05). In contrast, 30 patients enrolled on the low-touch IHPC program had no significant changes in the frequency of ER visits, inpatient admissions, or 30-day readmissions throughout the study window. Average symptom scores from the ESAS were statistically equivalent across the two models of care, excluding items related to overall wellbeing and appetite. The percentage of goal-scores met for pain, dyspnea, and anxiety were similar in both IHPC models.
Conclusions
A high-touch IHPC model can substantially lower healthcare costs, even after patients are discharged from the program. While a low-touch IHPC model does not offer the same cost-savings, it does provide generally equivalent levels of symptom management and goal-oriented care.
Implications
Health Systems and Managed Care Organizations should be cognizant of the lucrative value-proposition offered by high-touch IHPC, especially as healthcare continues moving towards value-based payment. The low-touch IHPC model is well suited to provide high-quality care, but may need to offer a greater spectrum of services to match the cost-savings observed in the high-touch model.
Author
Saad Akhtar, MBA
Medical Student
Albany Medical Center
47 New Scotland Ave
Albany, NY 12208