Creating a Financing Analysis Model for Pediatric Concurrent Care: A Pilot Study
Background
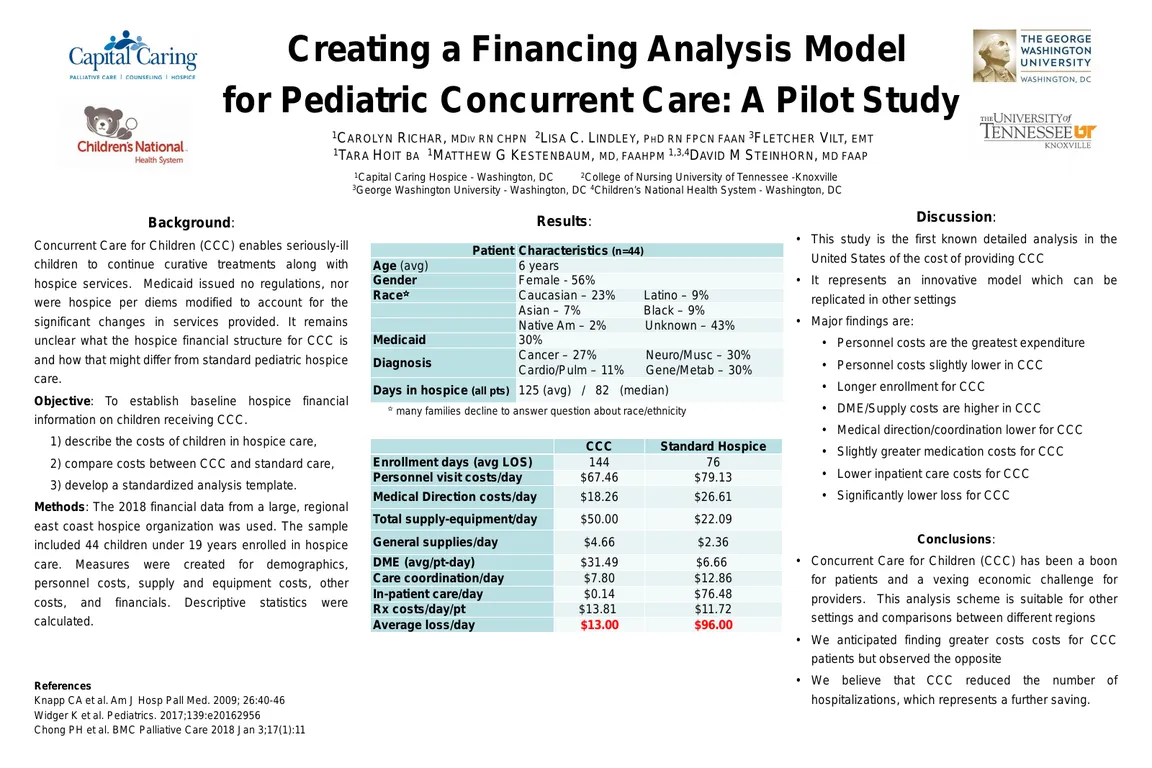
Concurrent Care for Children Requirement (CCCR) was enacted in 2010 with the passage of the Patient Protection and Affordable Care Act (Section 2302). CCCR enables seriously-ill children to continue curative treatments, while enrolled in Medicaid/CHIP hospice care with a <6-month life expectancy. Upon enactment of CCCR, Medicaid issued no regulations, nor were hospice per diems modified to account for the significant changes in services provided. Although CCCR has been in place for almost a decade, it remains unclear what the hospice financial structure is and how that might differ from standard pediatric hospice care.
Objective
The study purpose was to establish baseline hospice financial information on children receiving CCCR. The study aims were to: 1) describe the costs of children in hospice care, 2) compare costs between concurrent care and standard hospice care, and 3) develop a standardized analysis template.
Methods
The 2018 financial data from a large, regional east coast hospice organization was used. The sample included 44 children under 19 years enrolled in hospice care. Measures were created for demographics, personnel costs, supply and equipment costs, other costs, and financials. Descriptive statistics were calculated.
Results
The average age was 6 years. Fifty-six percent of children were females. Unknown (34.09%) and Caucasian (22.73%) were the most common and Native American (2.27%) the least common race/ethnicity. Approximately 1/3 had Medicaid insurance and a cancer diagnosis. The average hospice enrollment was 125 days (median = 82 days). CCCR children had an average enrollment of 144 days versus 76 days among non-CCCR children. Comparing CCCR and non-CCCR children, the average total costs of personnel visit were higher among non-CCCR children ($67.46/day vs. $79.13/day). Hospice medical director costs were higher among the children without CCCR ($26.61/day vs. $18.26/day) than those with CCCR. Total supply and equipment costs were higher for CCCR ($50.00/day) versus non-CCCR children ($22.09/day). General supplies were twice as high for CCCR children ($4.66/day vs. 2.36/day), while medications were similar between the groups. The cost of durable medical equipment was almost 5 times higher for CCCR children versus their peers. Although triage costs were similar between concurrent and non-concurrent children, care coordination ($7.80/day vs. $12.86/day) and inpatient care ($0.14/day vs. $76.48/day) costs were significantly higher for children without CCCR. Overall, children in hospice care incurred on average $161.10/day in direct and $44.43/day in administrative costs. Revenues averaged $169/day for all children. Between the groups, children without CCCR had twice the direct and administrative costs of CCCR children, while revenues were consistent. The average daily financial loss was ~$36.00/day for any child, ~$13.00/day for CCCR, and ~$96.00/day for those without CCCR.
Conclusions
Children in CCCR had longer hospice enrollments and incurred higher costs for general supplies and durable medical equipment, whereas non-CCCR children had higher costs for hospice medical director visits and inpatient care that incurred more care coordination costs. Although, the hospice organization experienced an average daily loss in caring for children, the financial loss was significantly less for CCCR children.
Author
Lisa C. Lindley, PhD, RN, FPCN
Associate Professor
University of Tennessee, Knoxville
College of Nursing
1200 Volunteer Blvd.
Knoxville, TN 37996
(865) 974-0653