Expanding the Interdisciplinary Team to Address Complex Social Needs
As a community-based palliative care program serving an urban Medicaid population, the Advanced Illness Care team takes care of patients disproportionately affected by poverty, housing instability, food insecurity, behavioral health conditions and substance use disorder.
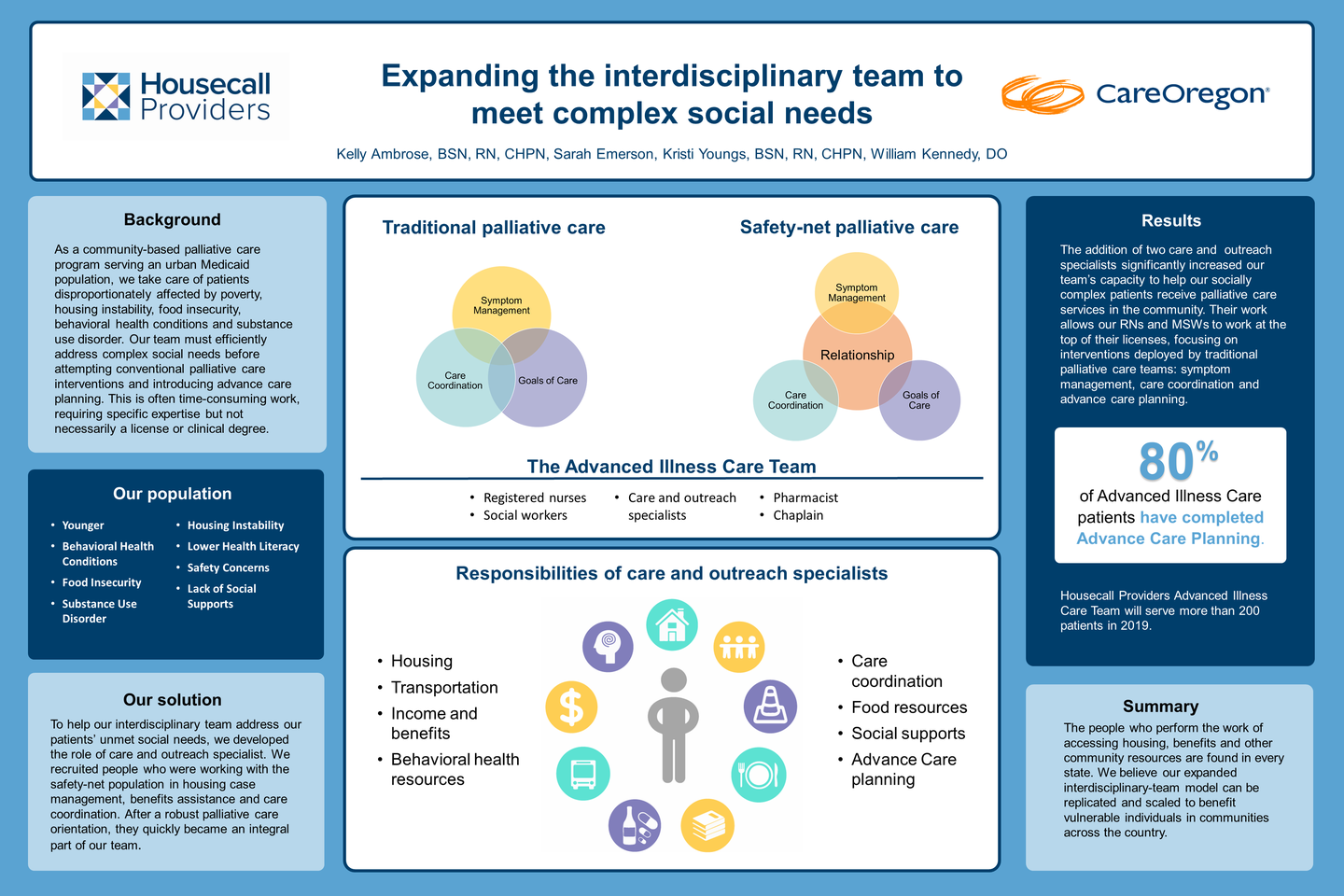
Our team must efficiently address complex social needs before attempting conventional palliative care interventions and introducing advance care planning. Symptom management, care coordination and discussing goals of care achieve little if a patient is worried about finding or maintaining housing, securing benefits, or simply trying to arrange transportation or child care for their next appointment. The maze of phone calls, forms and follow-up would challenge the most privileged among us — and is considerably more challenging for vulnerable individuals who are facing serious illness.
Helping patients deal with the effects of social determinants of health is often time-consuming work, requiring specific expertise – but not necessarily a license or clinical degree. To help our interdisciplinary team address our patients’ unmet social needs, we developed the role of care and outreach specialist. We recruited people who were working with the safety-net population in housing case management, benefits assistance and care coordination. After a robust palliative care orientation, they quickly became an integral part of our team.
The addition of two care and outreach specialists significantly increased the team’s capacity to help our socially complex patients receive palliative care services in the community. By meeting patients where they are and addressing basic needs, we earn their trust and quickly establish rapport. Their work allows our RNs and MSWs to work at the top of their licenses, focusing on interventions deployed by traditional palliative care teams: symptom management, care coordination and advance care planning. More than 80% of our patients have completed advance care planning; 34% have transitioned to hospice over the prior 12 months. Most importantly, we know we have improved the quality of each patient’s life at the end of their life.
The people who perform the work of accessing housing, benefits and other community resources are found in every state. We believe our expanded interdisciplinary team model could be replicated and scaled to benefit vulnerable individuals in communities across the country.
Author
Kelly Ambrose, BSN, RN, CHPN
Advanced Illness and Palliative Care Manager
Housecall Providers
5100 SW Macadam Ave, Suite 200
Portland, OR 97239
(971) 202-5504