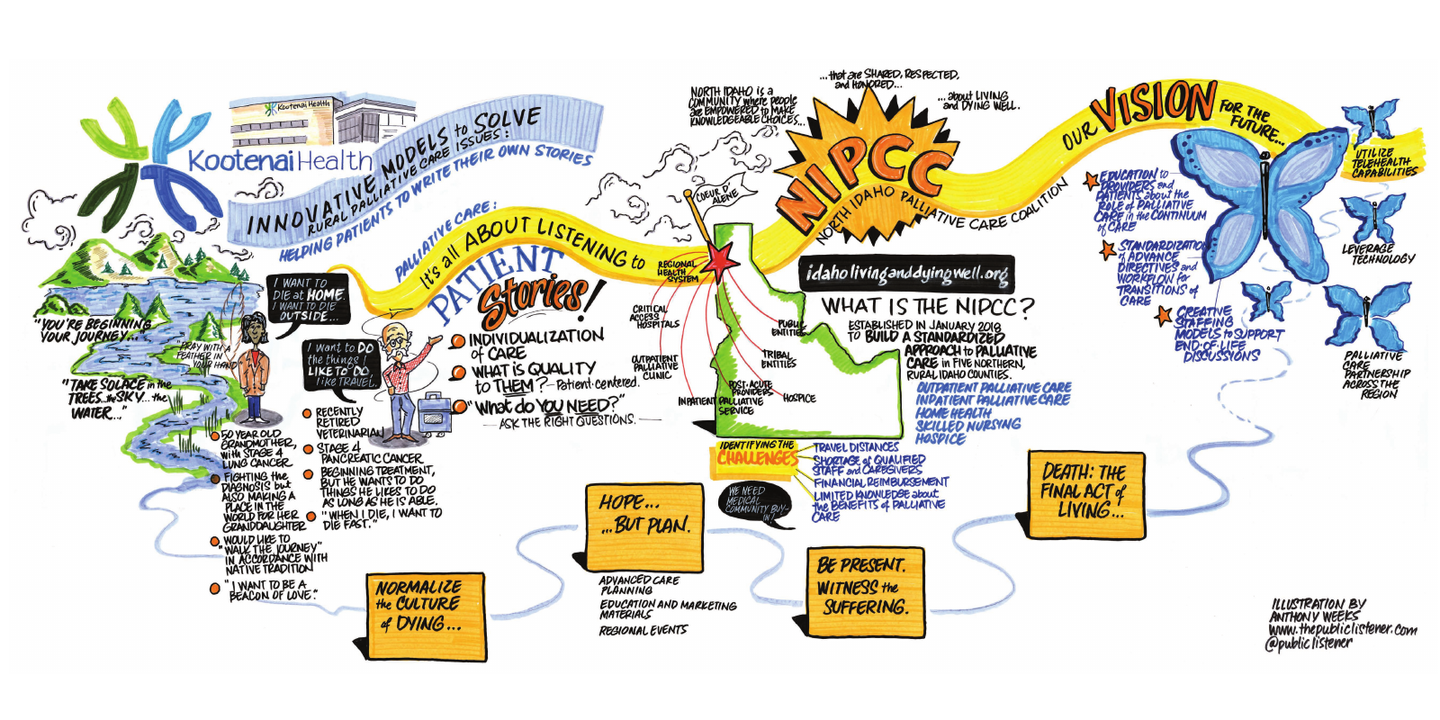
Innovative Model to Solve Rural Palliative Care Issues
In rural northern Idaho, providing palliative care is challenging due to travel distances, shortage of qualified staff and caregivers, financial reimbursement, and limited knowledge about palliative care and its benefits. The North Idaho Palliative Care Coalition (NIPCC) was established in January 2018 to build a standardized approach to palliative care in 5 rural northern Idaho counties. NIPCC is comprised of a diverse group of community partners including a community-owned regional health system, 4 critical access hospitals, post-acute providers, outpatient/inpatient palliative care and hospice services. The program has been extended to other community partners including tribal and public health entities.
The NIPCC mission statement states: North Idaho is a community where people are empowered to make knowledgeable choices that are shared, respected and honored about living and dying well.
Three areas of focus were identified for NIPCC:
1) Education to providers and patients about the role of palliative care in the continuum of care;
2) Standardization of advance directives and workflow for transitions of care;
3) Creative staffing models to support end-of-life discussions.
An educational program for physicians in the region was provided by CORE Training in partnership with The University of Washington Cambia Palliative Care Center of Excellence. This training was focused on complex medical conversations and symptom management. Feedback from participants was favorable and educational trainings are ongoing.
A concise advanced directive form was developed with input from a group of regional multidisciplinary physicians and patient representatives. The overarching goal was to ensure patient preferences for end of life care was honored across the region in a standard way.
A network of trained facilitators from the community was created to conduct advanced care planning conversations as an alternative staffing model. A new website serves as a centralized location for the custom advanced directive form, education and marketing materials, and calendar for coordinated regional events for health professionals and the public.
Areas of growth include utilizing telehealth capabilities and leveraging technology to offset geographic limitations of the rural area and ensure palliative care partnership across the region for the benefit of our patients.
Author
Jill Marie. Weeks, RN, MPH, MHCDS
Executive Director Transitional Care Services
Kootenai Health
2003 Kootenai Health Way
Coeur d'Alene, ID 83854
(208) 625-4309