Supporting Patients with Serious Illness to Plan Ahead
Planning ahead includes:
- Advance care planning
- Personal care and living arrangements
- Legal and financial planning
- Work and retirement planning
- Focusing on the 4Ms: What Matters, Mentation, Mobility, and Medications
Advance Care Planning
If planning is left until late stages of disease or near the end of life, it will be too late for many patients to participate (e.g., in the case of dementia, and/or the high prevalence of cognitive impairment due to the burden of any progressive serious illness).
Planning should occur soon after the diagnosis of a serious illness and be revisited periodically as illness progresses. This will maximize meaningful participation by the person while they retain decision-making capacity.
Planning ahead can help to ensure that values and preferences are known and followed. One of the most stressful parts of caregiving is the need to make decisions for a loved one while under time pressure (e.g., during a crisis) or without guidance about what the patients wants.
Advance care planning is a longitudinal process in which individuals:
- Identify someone who should make decisions for them if they cannot
- Think about their personal values and goals
- Consider what types of care they would or would not want in different medical situations
- Discuss their preferences with their loved ones and clinicians
- Ask: “If sometime in the future, you were to have brain damage severe enough that you could no longer recognize or interact with your family and loved ones, what should we prioritize? Would you want your care to focus primarily on your comfort at that point in your life, or would you prefer to continue all life-prolonging treatments?”
Be aware of available advance care planning training.
Personal Care and Living Arrangements
A person with serious illness, and their family, should start putting a plan in place for personal care and long-term care. This might include identifying financial resources (e.g., long-term care insurance), family or paid caregivers, and community resources.
Identify which friends, family, and neighbors may be willing to help as the disease progresses, recognizing that caregiving responsibilities often require more than one person.
Legal and Financial Planning
Clinicians do not need to be financial planning experts, but they can help focus the patient and family on its importance and refer patients and families to community resources for financial planning assistance.
Work and Retirement Planning
Some patients find that working helps them feel better both physically and emotionally. Others feel differently. The key is to allow time for individuals to consider any possible implications of work-related decisions, including:
- Risks to safety associated with working
- The ability of the company to provide support and accommodation
- The possibility of changing or reducing duties
- Effect on benefits and other entitlements
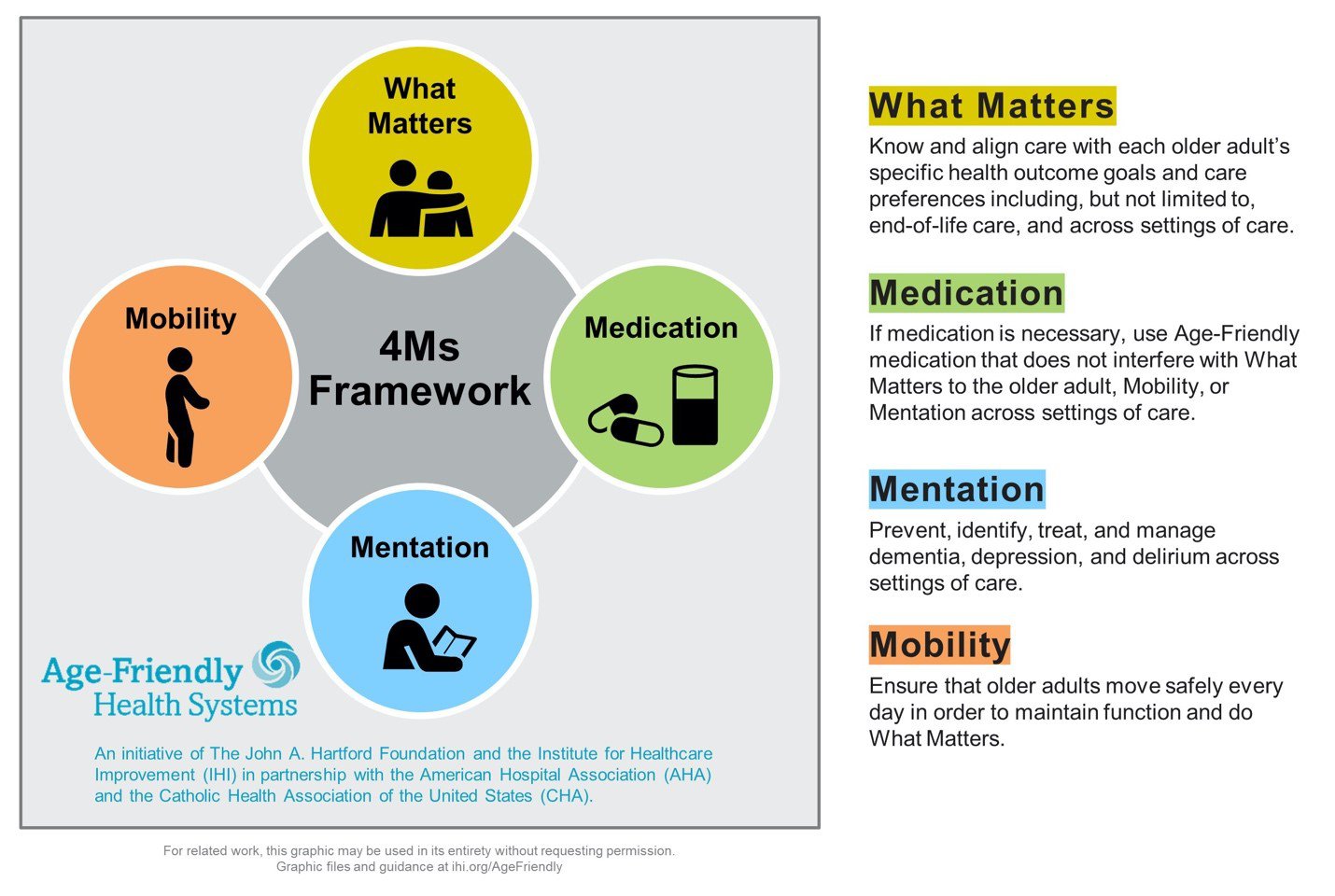
Using the 4M’s Framework
All older adults and all people living with a serious illness require care informed by the principles of prevention and mitigation of common hazards associated with both the illness itself, and with the unintended consequences of medical care and medications. Using the 4Ms Framework serves as a structured reminder of the importance of reducing risks to cognitive and functional independence, which is, by far, the highest priority of patients in multiple studies.
What Matters: Know and align care with each older adult's specific health outcome goals and care preferences including, but not limited to, end-of-life care, and across settings of care.
Medication: If medication is necessary, use Age-Friendly medication that does not interfere with What Matters to the older adult, Mobility, or Mentation across settings of care.
Mentation: Prevent, identify, treat, and manage dementia, depression, and delirium across settings of care.
Mobility: Ensure that older adults move safely every day in order to maintain function and do What Matters.